Referral and Prior Authorizations in Medical Billing: How to Avoid Denials
Referral and prior authorizations in medical billing are one of the biggest headaches for healthcare providers. But like it or not, they’re part of the job.
If you don’t handle them correctly, you’ll run into problems—delays in care, denied claims, and frustrated patients. The good news? You can simplify the process.
In this post, we’ll show you how to manage prior authorizations and referrals without the chaos.
Table of Contents
Key Takeaways:
- Prior authorizations are mandatory approvals for services but don’t guarantee full coverage.
- Referrals differ in that they approve specialist visits, not services or procedures.
- Missing details like authorization numbers can cause denials.
- Use EMR/EHR systems or manual tracking tools to avoid missed authorizations or expired referrals.
- Assign dedicated staff to handle prior authorizations and referrals efficiently.
- Know your payors’ unique rules to avoid unnecessary delays and confusion.
- Educate patients about the limits of prior authorizations to reduce billing disputes.
What Are Prior Authorizations in Medical Billing?
At their core, prior authorizations are formal approvals from an insurance company for certain services, prescriptions, or procedures before they’re provided. The idea is that the insurance company wants to make sure what you’re requesting is medically necessary and worth the expense. It’s their way of micromanaging—sorry, I mean “regulating”—your care decisions. This adds a whole extra layer of hassle for providers, as these approvals aren’t optional; they’re required if you want the insurance to cover the service.
Here’s the short version: no prior authorization, no coverage.
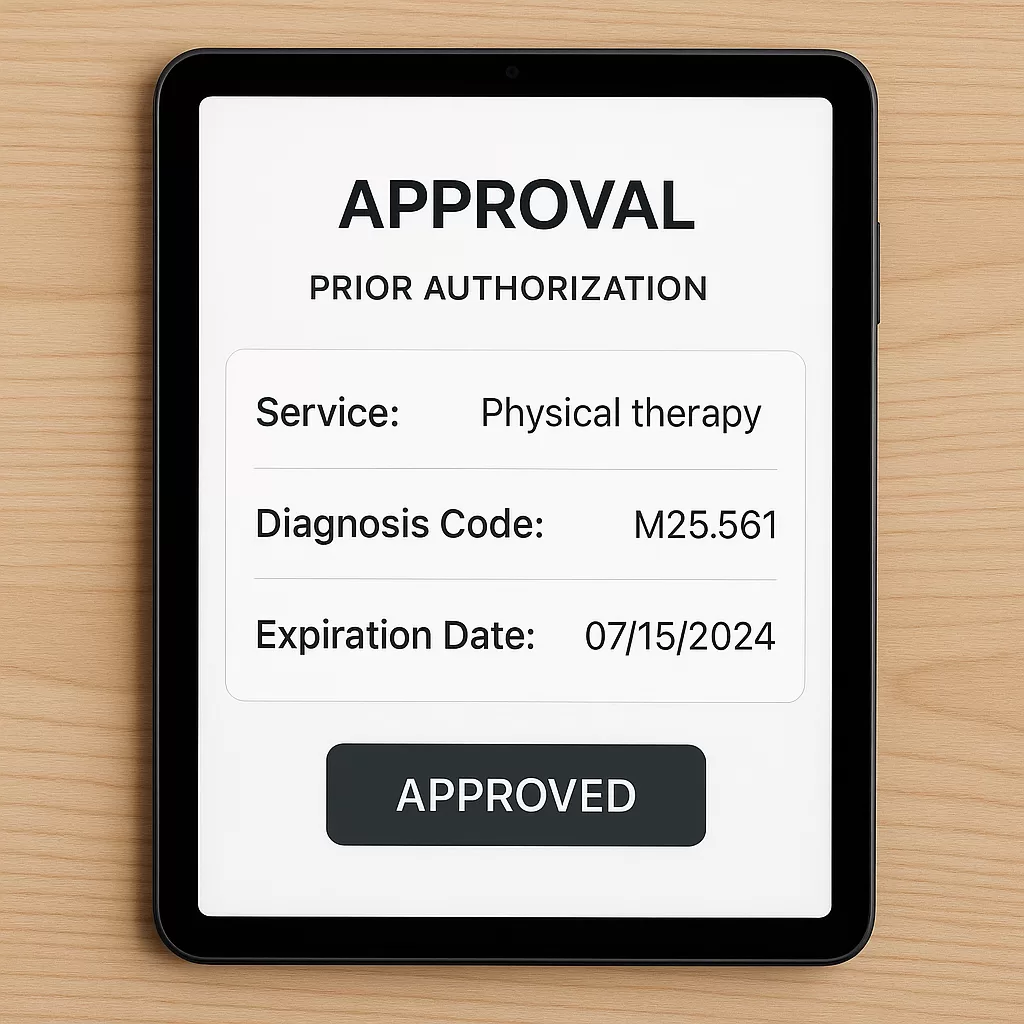
Now, these authorizations aren’t just a vague “yes” from the insurance company. They’re tied to specifics:
- What’s being approved (medication, imaging, service, etc.)
- Why it’s being approved (specific diagnosis codes or steps in treatment).
- For how long it’s valid (30 days? 60 days? Maybe 90 if you’re lucky).
You’ll often need to supply detailed information, like the patient’s medical history, diagnostic codes, or proof that other treatments have failed. The insurance company may then deny the request (cue the groans), in which case the provider has to appeal, send more documentation, or even call them directly to fight for approval.
What’s the Billing Impact of Prior Authorizations?
Once you’ve jumped through all the hoops and the insurance company begrudgingly grants you a prior authorization number, you’re not yet off the hook. This approval comes with very specific billing requirements. If you don’t follow them, your claim will be denied faster than a kid trying to use Monopoly money at a vending machine.
Key Billing Requirements and Mistakes to Avoid
- Include the authorization number: Your insurance claim has a designated space for the prior authorization number. Forgetting to include this is guaranteed to result in denial.
- Pay attention to time frames: The approved service must occur within the authorized dates. If you try to bill for something outside the approval window, it’s like the authorization never existed.
- Patient misconceptions: Many patients think prior authorization equals full coverage. Spoiler: it doesn’t. That medication could still cost them hundreds of dollars, or the imaging could go toward their deductible. Ensure your patients understand this upfront to avoid confusion (and angry phone calls).
How Do Referrals Differ From Prior Authorizations?

If you’ve been paying attention, you might think, “Wait, this sounds a lot like referrals.” And you’d be right—referrals are similar, but they’re not the same.
Referrals are usually required for patients to see specialists, while prior authorizations approve specific services. See the table below for a full comparison.
For example, many HMO plans require patients to get a referral from their primary care doctor before seeing a specialist. The referral might authorize a certain number of visits (e.g., five visits within six months) or cover all visits for a calendar year.
Comparison Table – Referrals vs Prior Authorizations
| Feature | Prior Authorization | Referral |
|---|---|---|
| Purpose | Approval for services or procedures | Approval to see a specific provider |
| Who Requests It | Usually, the patient’s primary care doctor | Usually the patient’s primary care doctor |
| Approval Details | Linked to specific services and time frames | Often allows multiple visits over time |
Both are annoying, yes, but referrals tend to be more flexible regarding time frames and are usually easier to renew.
How to Track Referrals and Prior Authorizations Efficiently
Alright, now that we’ve covered prior authorizations and referrals, let’s talk about how to handle them without letting them take over your entire practice. It’s all about having the right workflow, tools, and—most importantly—the right people to keep the machine running smoothly. Whether it’s tracking approvals, avoiding denials, or keeping communication flowing, these tips will save you from a world of frustration.
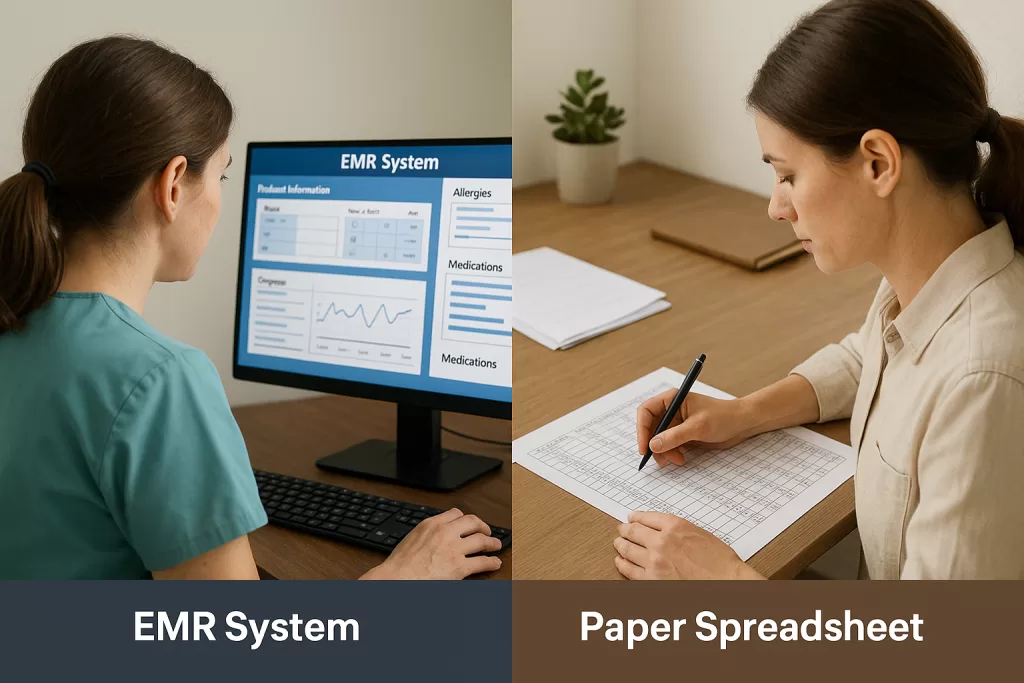
Best Tools: EHR, Spreadsheet, or Specialist?
One of the biggest challenges with prior authorizations and referrals is ensuring nothing falls through the cracks. If you’re not tracking approvals and time frames, it’s only a matter of time before you get hit with a denied claim—and trust me, appealing these denials is like trying to untangle a pair of headphones from the bottom of your bag.
Options for Tracking Prior Authorizations and Referrals:
- EMR/EHR Systems:
Many electronic medical records (EMR) or health record (EHR) systems have built-in tools to track prior authorizations and referrals. You can usually set up alerts for expiration dates, monitor approval statuses, and link authorization numbers directly to claims. - Manual Tracking:
If your EMR doesn’t support authorization tracking (or doesn’t have an EMR system), you’ll need to track them manually. This could mean spreadsheets, calendars, or shared docs. Sure, it’s less fancy, but it works—just make sure it’s accessible to the whole team and regularly updated. - Dedicated Staff:
Some practices hire a referral specialist or prior authorization specialist whose sole job is managing approvals, tracking visits, and handling renewals. If you’re in a high-volume practice, this person could save you thousands of dollars in denied claims.
What Should You Track to Avoid Denials?
- Authorization Numbers: Include them on every relevant claim.
- Approval Dates: Ensure services are scheduled within the authorized time frame.
- Visit Limits: For referrals, count the number of visits used and the number left.
Here’s a simple table you can use for tracking:
| Patient Name | Authorization Type | Number | Service/Visits Approved | Time Frame | Remaining Visits |
|---|---|---|---|---|---|
| Jane Doe | Prior Authorization | 123456789 | MRI | Jan 1, 2024 – Feb 1, 2024 | N/A |
| John Smith | Referral | 987654321 | 5 office visits | Jan 1, 2024 – Dec 31, 2024 | 3 |
Who Handles Referrals and Authorizations in a Medical Practice?
Now, let’s talk about workflow. In any practice, there needs to be a clear chain of responsibility when it comes to prior authorizations and referrals. If everyone assumes “someone else” is taking care of it, you’re headed straight for disaster.
Key Roles and Responsibilities by Department
- Front Office Staff:
They’re often the first point of contact, so they should be trained to know when a prior authorization or referral is required. If the patient’s insurance requires one, the staff should flag it before scheduling the service. - Referral Specialist:
In larger practices, having a dedicated referral specialist can streamline the entire process. This person obtains prior authorizations, tracks approvals, and communicates with the billing team. - Billing Team:
Once services are provided, the billing team is responsible for ensuring that the correct prior authorization or referral number is included on claims. They also handle denials, so they should work closely with the front office to ensure no errors occur upfront.
What to Do If Something Goes Wrong With an Authorization

Even with the best systems in place, mistakes happen. Maybe a prior authorization wasn’t obtained, or the referral expired before the patient was seen. When this happens, you need to act quickly to minimize the impact.
Steps to Correct Denials and Prevent Future Issues
- Identify the Issue:
Look at the explanation of benefits (EOB) or ERA (Electronic Remittance Advice) to see why the claim was denied. If it says “No prior authorization on file,” you know what went wrong. - Backtrack:
Find out what services were provided, the patient’s insurance plan, and whether prior authorization is required. - Appeal or Request Retro Approval:
Some insurance companies will allow you to request retroactive approval if you prove the service was medically necessary. But keep in mind that this is becoming less common. - Prevent Future Errors:
Use the denial as a learning opportunity. Update your internal process or tracking system to prevent it from happening again.
Why Knowing Your Payors’ Rules Matters
Each insurance company has its own rules when it comes to prior authorizations and referrals. Some HMOs are sticklers for referrals, while others are lenient. The best way to avoid issues is to have someone in your practice who understands the nuances of your major payors.
For example:
- Insurance A might require prior authorization for MRIs, but not CT scans.
- Insurance B could require referrals for every specialist visit, no exceptions.
If you know the quirks of each insurance plan, you can set your practice up for success—and avoid surprises.
FAQ: Referral and Prior Authorizations in Medical Billing
What are prior authorizations?
Prior authorizations are formal approvals insurance companies require for certain medical services, procedures, or prescriptions before they are provided. These approvals ensure the service is deemed medically necessary and covered under the insurance plan. The service may not be covered without prior authorization, leading to denied claims.
Why are prior authorizations necessary?
Insurance companies use prior authorizations to regulate healthcare costs and ensure treatments are medically necessary. Providers must submit documentation, like diagnostic codes and patient history, to justify the service. This process prevents unnecessary expenses but often adds administrative burdens to providers and delays patient care.
What happens if I don’t get prior authorization?
Without prior authorization, insurance will likely deny coverage for the service, leaving the patient responsible for the full cost. Additionally, denied claims can create financial and administrative challenges for the practice, requiring appeals or retroactive approval requests, which may not always succeed.
How do referrals differ from prior authorizations?
Referrals are approvals from a primary care provider for a patient to see a specialist, often required by HMO plans. Unlike prior authorizations, which approve specific services, referrals typically authorize a certain number of visits within a set timeframe and are usually easier to obtain.
Why do patients often misunderstand prior authorizations?
Many patients assume prior authorization guarantees full coverage, but it only ensures the service is approved for insurance purposes. Patients may still face costs like copayments, deductibles, or uncovered portions of the bill. Clear communication from the practice can help avoid confusion and frustration.
How can practices streamline prior authorization and referral workflows?
Practices can streamline workflows by using EMR/EHR systems with tracking features, employing manual tracking tools like spreadsheets, or designating staff members to manage approvals. Proactively tracking expiration dates, approval statuses, and visit limits can help avoid denied claims and keep operations efficient.
What are the billing requirements for prior authorizations?
It’s crucial to include the prior authorization number on claims, ensure services occur within the authorized time frame, and verify that all billing codes match the approved procedure or service. Failing to meet these requirements can result in claim denials.
What should practices track for prior authorizations and referrals?
Practices should track authorization numbers, approval dates, service timeframes, and visit limits. A detailed tracking system ensures that services are scheduled and billed accurately, minimizing the risk of denials and reducing administrative workload.
What should I do if a claim is denied due to missing prior authorization?
First, review the explanation of benefits (EOB) to identify the reason for the denial. Then, verify if prior authorization was required and obtained. If not, appeal the denial or request retroactive approval if allowed. Use the incident to update workflows and prevent future errors.
Who is responsible for handling prior authorizations in practice?
Responsibility is often shared between front office staff, referral specialists, and the billing team. Front office staff flag necessary authorizations, specialists handle approvals, and the billing team ensures claims include authorization numbers. Clear role definitions help prevent errors and streamline the process.
How can I educate patients about prior authorizations and referrals?
Provide patients with a brief explanation of prior authorizations and referrals, emphasizing that approval does not guarantee full coverage. Educating patients upfront reduces confusion, improves satisfaction, and minimizes follow-up calls about unexpected costs or denied claims.
Take Control of Referrals and Authorizations in Your Practice

Let’s face it—prior authorizations and referrals are the unsung villains of every medical practice. They’re time-consuming, confusing, and can make you feel like you’re in a never-ending battle with insurance companies. But with the right systems, workflows, and a proactive team, you can turn this headache into a manageable part of your day-to-day operations.
To recap:
- Prior authorizations ensure that high-cost services and prescriptions are approved before they’re performed—but they don’t guarantee full coverage for the patient.
- Referrals are necessary for patients to see specialists and may be tied to specific time frames or visit counts.
- Both processes require careful tracking, communication, and the inclusion of authorization numbers on claims to avoid costly denials.
- Establish a streamlined workflow in your office that identifies who’s responsible for requesting, tracking, and including these authorizations on claims.
The key is to stay organized, proactive, and informed about what’s required for each insurance plan and each service. Mistakes happen, but with a solid system, you’ll minimize those errors, avoid denials, and keep your practice running smoothly.
If this all feels overwhelming, don’t sweat it—start small. Even a basic spreadsheet can be a game-changer if you don’t have a fancy EMR system. And don’t forget to educate your patients, too. A quick explanation of what prior authorizations and referrals mean can save you from endless phone calls later when they receive their bill and wonder why it’s not “free.”
The bottom line? Prior authorizations and referrals might feel like hurdles, but with the right processes, you can jump over them like a billing pro.
Thanks for sticking around! If you have questions, stories, or tips about prior authorizations and referrals, drop them in the comments below—I’d love to hear from you.