Top Five Credentialing Mistakes and How to Avoid Them
Credentialing mistakes can wreak havoc on an already time-consuming process. Even seasoned pros stumble over details, leading to delays and rejections. In this guide, I’ll highlight the top 5 credentialing mistakes that create headaches for providers and practices—and share tips to streamline your process.
Let’s jump into it!
1. Submitting Incomplete Applications
The number one credentialing mistake is submitting incomplete applications. You might think, “This seems basic—how do people mess it up?” But trust me, it happens all the time.
An application missing even one piece of required information will be sent back by the insurance company—no questions asked. Insurance companies don’t want to chase you down for missing details. Instead, they reject the application outright, and you’re back to square one.
Why is this such a big deal? Because credentialing timelines are long enough as it is. Starting over from scratch delays the process significantly, especially if you’re working with a slow-moving payer.
Pro Tip:
If you’re just starting out, or even if you’ve been doing this for a while, make it a habit to double-check every single field. In my advanced credentialing course, we walk through a full credentialing application line by line to ensure nothing gets missed.
Key takeaway? Leaving blanks = rejection.
2. Providing Incorrect Information
If mistake #1 is leaving things blank, mistake #2 is just as damaging: submitting incorrect information.
Let’s say you fill out the application entirely—but the data you entered is wrong or doesn’t match the insurance company’s records. Guess what? They’re going to reject it anyway.
Here’s what happens:
- Insurance companies cross-check the information you submit with their records.
- If there’s a mismatch, the application gets flagged and sent back.
Sometimes, payers will allow you to resubmit the correct information without penalty. But other times? You’re back at the end of the line, and you’ve just added weeks (or months) to the credentialing process.
Common problem areas include:
- Provider names that don’t match exactly (e.g., missing middle names).
- Incorrect NPI numbers (which brings us to mistake #3).
- Address or group affiliation errors.
Bottom line? Always triple-check the details before submitting. Even one small error can send you back to square one.
3. Confusing NPI 1 and NPI 2
Understanding NPI 1 vs. NPI 2 is critical for credentialing success, yet many people get tripped up about this.
- NPI 1: This is the individual provider’s NPI. It’s specific to the individual and follows them throughout their career.
- NPI 2: This is the group or organization’s NPI. It’s tied to the practice, not the provider.
Here’s why this matters: When submitting applications or claims, you need to make sure the right NPI is entered in the right place. If there’s a mismatch—say, you accidentally enter the NPI 2 in a field that’s supposed to have the NPI 1—it will create problems.
What happens when you mix these up?
- Insurance companies will reject the claims.
- You’ll have to resubmit and potentially return to the credentialing queue’s start.
- It can cause delays and financial headaches for the provider or group.
Quick Tip:
Think of the NPI 1 as the “who” (individual) and the NPI 2 as the “where” (organization). Keeping these straight is non-negotiable in the credentialing process.
4. Failing to Prioritize Applications
If you’re not prioritizing your credentialing applications, you’re setting yourself up for delays and frustration.
Not all payers are created equal. Some credentialing timelines are significantly longer than others. For example:
- Government payers like Medicare, Medicaid, and Tricare are notoriously slow. These applications should always be prioritized first.
- Commercial payers like Blue Cross Blue Shield, UnitedHealthcare, and Aetna tend to move faster but can still take months to process.
If you start with the wrong applications—like smaller, local plans—and leave the slowest payers for last, you could find yourself in a bind.
5. Lack of Organization
The fifth and final credentialing mistake is not being organized. If you’re disorganized, you’re setting yourself—and your providers—up for failure.
Here’s the reality: Credentialing is all about attention to detail and keeping track of multiple moving parts. Without an organized system, it’s easy to lose track of deadlines, application statuses, and key pieces of information.
What happens when you’re disorganized?
- Applications get submitted late or not at all.
- You provide outdated or incomplete information.
- You miss critical follow-ups, which delays the entire process.
This is especially problematic for credentialing specialists. Whether you’re in-house at a practice or a third-party professional hired to manage credentialing, your job is to keep the process smooth and timely. Delays caused by disorganization aren’t just inconvenient—they cost the provider money.
Imagine this:
A provider hires you to credential them with a major payer. You fail to follow up on the application for weeks, and the process drags on longer than it should. Because of the delay, the provider isn’t reimbursed for services they’ve already rendered. That’s money lost—and it’s entirely preventable.
How to stay organized?
- Use a reliable tracking system (spreadsheets, software, or project management tools).
- Take clear, consistent notes about each payer’s requirements and timelines.
- Regularly update the provider or organization on the status of each application.
Organization and attention to detail are the two pillars of credentialing success.
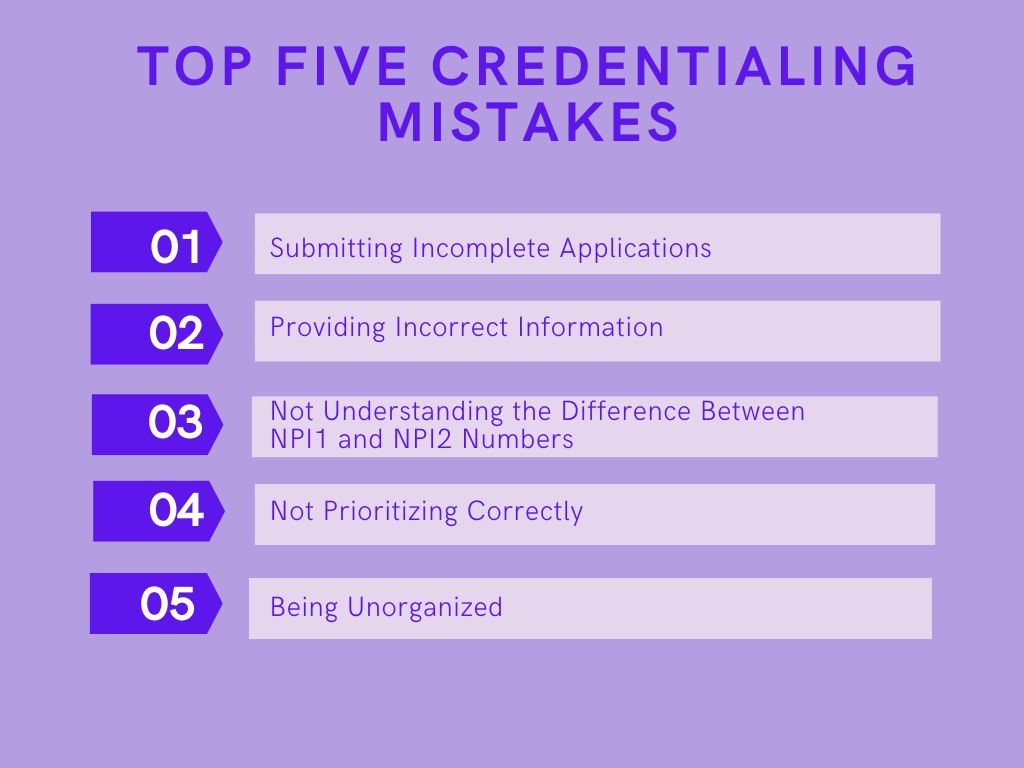
Quick Recap: The Top 5 Credentialing Mistakes
Let’s quickly go over the five biggest credentialing mistakes that can derail the process:
- Submitting incomplete applications – Missing information = instant rejection.
- Providing incorrect information – Errors cause delays and can send you back to square one.
- Confusing NPI 1 and NPI 2 – Mixing these up will result in claim rejections and credentialing setbacks.
- Failing to prioritize applications – Always tackle the slowest payers (like government plans) first.
- Lack of organization – Disorganization leads to delays, lost money, and frustrated providers.
If you avoid these five mistakes, you’ll save time, stress, and headaches throughout the credentialing process.
Take Your Credentialing Skills to the Next Level
If you’re ready to master the credentialing process, I’ve got you covered. My Healthcare Credentialing and Contracting Course is available through the Thinkific platform. It’s broken down into three sections:
| Level | Who It’s For | What You’ll Learn |
|---|---|---|
| Beginner | New to credentialing | Step-by-step basics to get started successfully |
| Intermediate | Those with some experience | Refining processes, avoiding common mistakes |
| Advanced | Seasoned pros looking to level up | Deep dive into applications, line-by-line reviews, and strategy |
Each section is:
- Self-paced – No deadlines or expiration dates.
- Flexible – Depending on your needs, you can choose one section or all three.
- Comprehensive – Includes overview videos and resources for every lesson.
FAQ
What are the most common credentialing mistakes?
The most common credentialing mistakes include submitting incomplete applications, providing incorrect information, confusing NPI 1 and NPI 2, failing to prioritize payers, and lacking organization. Avoiding these pitfalls can help streamline the process and prevent unnecessary delays.
Why is submitting incomplete credentialing applications such a problem?
Submitting incomplete applications leads to immediate rejections by payers. Even one missing detail will force you to start over, significantly delaying timelines. To avoid this, double-check every field on the application to ensure accuracy and completeness before submission.
How does providing incorrect information affect credentialing timelines?
Incorrect information, such as mismatched names or wrong NPI numbers, causes delays because insurance companies cross-check submissions. Applications flagged for errors are either returned for correction or rejected entirely, forcing you to resubmit and adding weeks—or even months—to the process.
What is the difference between NPI 1 and NPI 2?
NPI 1 is for individual providers, following them throughout their careers. NPI 2 is for organizations or groups. Confusing these can result in rejected claims and setbacks. Always ensure you input the correct NPI in the proper fields during credentialing.
Why is it important to prioritize credentialing applications?
Prioritizing applications ensures the slowest-moving payers, such as Medicare and Medicaid, are submitted first. These government plans often have long timelines, so delaying them can cause reimbursement issues and frustration for providers waiting to begin billing.
How can disorganization impact the credentialing process?
Disorganization can lead to missed deadlines, incomplete applications, and failure to follow up. This delays credentialing and costs providers money if they cannot bill payers on time. Using tracking systems and organized workflows is essential for success.
How can I avoid credentialing delays caused by common mistakes?
To avoid delays, double-check applications for completeness, verify all details for accuracy, understand NPI 1 vs. NPI 2, prioritize slower payers first, and stay organized with a tracking system. Attention to detail is key to a smooth credentialing process.
Who can benefit from a credentialing course?
Anyone involved in provider credentialing can benefit, including beginners, intermediates, and advanced professionals. A structured course provides step-by-step guidance, process refinements, and strategies for avoiding common mistakes, making the process more efficient and effective.
What tools can help with credentialing organization?
Tools like spreadsheets, project management software, or dedicated credentialing platforms can help keep track of application statuses, deadlines, and payer requirements. Consistent note-taking and regular follow-ups are critical for maintaining organization and preventing delays.
How can I learn more about improving my credentialing process?
To improve your credentialing skills, consider enrolling in a comprehensive course, like the Healthcare Credentialing and Contracting Course on Thinkific. It covers basics to advanced strategies and offers flexible, self-paced learning to fit your needs.
Share Your Thoughts!
I’d love to hear from you:
- Have you run into these credentialing mistakes in your own experience?
- Are there other mistakes you think deserve a spot in the top five?
Drop your thoughts in the comments below, and let’s keep the conversation going!